The 1918 Influenza Pandemic, commonly known as the Spanish Flu, is one of the most devastating pandemics ever recorded in human history. Sweeping acr
The 1918 Influenza Pandemic, commonly known as the Spanish Flu, is one of the most devastating pandemics ever recorded in human history. Sweeping across the globe in the final years of World War I, it infected an estimated 500 million people—about one-third of the world’s population—and resulted in an estimated 50 million to 100 million deaths worldwide. This pandemic profoundly affected societies, public health, and medical science, shaping how the world responds to viral outbreaks even today. This article explores the origins, spread, impact, and aftermath of the 1918 influenza pandemic, while highlighting its lessons for modern public health.
The Emergence of the 1918 Influenza Virus
The pandemic was caused by an H1N1 influenza A virus, a subtype of influenza known to infect humans. Although scientists have not definitively pinpointed the exact place where the virus first emerged, multiple theories exist. Some researchers believe it started in the United States, possibly at a military base in Kansas, before spreading to Europe via troop movements. Others suggest the origin could be in France or China.
The rapid troop mobilization during World War I played a crucial role in the virus’s dissemination. Soldiers living in crowded barracks, trenches, and transport ships created ideal conditions for the virus to mutate and spread. The war’s disruption of daily life and infrastructure also hampered early containment efforts.
Why Was the 1918 Flu So Deadly?
Unlike typical seasonal influenza strains, the 1918 virus was unusually lethal and affected a broad range of age groups, including healthy young adults aged 20 to 40, a demographic usually resistant to severe flu complications.
One key reason for its lethality is thought to be a phenomenon called a “cytokine storm.” In this immune response, the body’s defense system overreacts to the infection, causing severe inflammation and tissue damage—especially in the lungs—leading to respiratory failure.
Victims often developed secondary bacterial pneumonia, a common cause of death during the pandemic. At the time, antibiotics were not yet discovered, so doctors had no effective treatment for these infections.
The Three Waves of the Pandemic
The 1918 influenza pandemic struck in three waves:
- First wave (spring 1918): This wave was relatively mild and similar to seasonal flu in symptoms and mortality. It mainly served as a warning sign of what was to come.
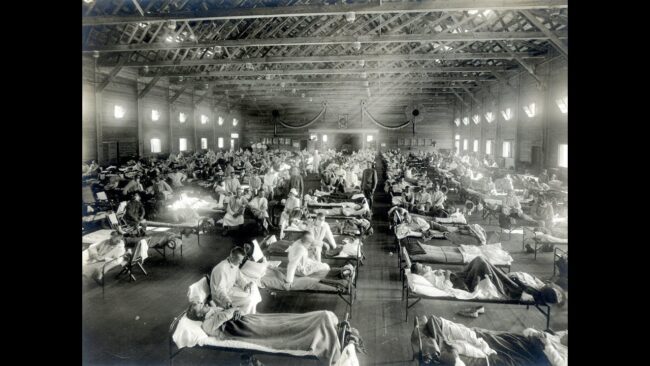
- Second wave (fall 1918): The deadliest phase, characterized by rapid onset and high fatality rates. In some locations, mortality reached as high as 10% of infected individuals. This wave overwhelmed hospitals and caused widespread panic.
- Third wave (winter 1918-1919): Less severe than the second, but still deadly. It caused renewed outbreaks globally and persisted into 1919 and early 1920 in some areas.
Global Spread and Impact
The pandemic spread worldwide, affecting every inhabited continent. It reached remote areas, including Pacific islands and Arctic regions. Some Indigenous populations, such as those in Alaska and Australia, experienced mortality rates much higher than average due to little prior exposure and limited access to medical care.
In the United States alone, an estimated 675,000 people died, and millions more fell ill. European countries, devastated by the war, also suffered catastrophic losses. Cities like Philadelphia experienced severe outbreaks, worsened by public gatherings that accelerated transmission.
Globally, the estimated death toll ranges between 50 million and 100 million, far exceeding the fatalities of World War I itself. The pandemic disproportionately affected young adults, a unique feature that contributed to a significant demographic and social impact.
Social and Economic Disruptions
The pandemic severely disrupted everyday life. Schools, theaters, churches, and businesses closed for weeks or months at a time. Public health authorities imposed quarantines, travel restrictions, and mask mandates to limit spread.
Economically, the loss of life and illness among working-age adults created labor shortages in key industries. Agricultural production, manufacturing, and transportation all suffered. This compounded the economic hardships already present due to the war.
The healthcare system was stretched beyond capacity. Medical staff faced shortages of supplies and personnel, and many healthcare workers themselves became ill or died. Funeral homes and cemeteries were overwhelmed by the sheer number of deaths.
Advances and Changes in Public Health
Though the virus could not be controlled by medical treatment at the time, the 1918 pandemic accelerated changes in public health policy and research:
- Disease Surveillance: The pandemic demonstrated the critical importance of timely disease reporting and international information sharing.
- Public Health Infrastructure: Many countries invested in building stronger health systems and creating organizations dedicated to epidemic prevention and control.
- Vaccine Research: The urgency of the crisis propelled influenza research, eventually leading to the isolation of the virus and vaccine development decades later.
- Pandemic Preparedness: Governments recognized the need for plans and resources to respond to future outbreaks.
These efforts laid the groundwork for improved responses to subsequent influenza pandemics and other infectious diseases.
Lessons for the Present and Future
The 1918 influenza pandemic offers enduring lessons that remain relevant today:
- Early Intervention Saves Lives: Swift implementation of social distancing, quarantines, and public health measures can slow viral spread and reduce mortality.
- Transparent Communication Is Crucial: Open, accurate information helps maintain public trust and compliance with health guidelines.
- Healthcare Systems Must Be Prepared: Adequate resources, personnel, and planning are essential for coping with surges in patients.
- Global Cooperation Matters: Viruses spread across borders, so international collaboration is vital for surveillance, research, and resource sharing.
- Vaccines and Treatments Are Game-Changers: Investment in vaccine development and antiviral drugs significantly reduces the impact of pandemics.
The COVID-19 pandemic of 2020 underscored the ongoing importance of these lessons and the need to continuously improve pandemic preparedness.
Conclusion
The 1918 Influenza Pandemic was a tragic milestone in global health history. It highlighted humanity’s vulnerability to infectious diseases but also spurred advances in medicine, public health, and international cooperation. Remembering the scale and severity of the 1918 pandemic helps ensure that future generations are better equipped to prevent and mitigate similar crises. The story of the Spanish Flu is both a cautionary tale and a testament to the resilience of humanity.
Frequently Asked Questions (FAQs)
Q1: Why was the 1918 flu called the “Spanish Flu” if it didn’t start in Spain?
A1: Spain was neutral during World War I and had no wartime censorship, so it openly reported on the flu outbreak. Many other countries suppressed information, making it appear as if Spain was hit hardest, though the virus was worldwide.
Q2: How many people died in the 1918 influenza pandemic?
A2: Estimates vary, but between 50 million and 100 million people died globally, making it one of the deadliest pandemics in history.
Q3: What made the 1918 influenza virus different from seasonal flu?
A3: It caused severe illness even in healthy young adults, likely due to an overactive immune response called a cytokine storm, which was rare in seasonal flu.
Q4: How did World War I influence the spread of the pandemic?
A4: Troop movements, crowded military camps, and poor sanitation facilitated rapid and global spread of the virus.
Q5: Were there any vaccines or treatments for the 1918 flu?
A5: No effective vaccines or antiviral treatments existed at the time. Medical care was mostly supportive, and antibiotics for secondary infections were not yet available.
Q6: What public health measures were taken during the pandemic?
A6: Measures included quarantines, social distancing, mask-wearing, school and business closures, and bans on public gatherings.
Q7: Did the pandemic have any long-term effects on medicine and public health?
A7: Yes, it led to improvements in disease surveillance, public health infrastructure, vaccine research, and pandemic preparedness.
Q8: Can pandemics like the 1918 flu happen again?
A8: Yes. While medical advances have improved preparedness, viruses can mutate, and pandemics remain a global risk requiring vigilance and cooperation.
For more info: infromednation


COMMENTS